Many patients have heard of the most common long-term effects of COVID-19: symptoms such as breathing issues, brain fog, and constant fatigue. But there is mounting evidence that COVID-19 may also affect sexual health negatively in both men and women. Men who hadn’t previously had problems of this nature have started developing erectile dysfunction (ED) after their COVID-19 infection.
In fact, studies show that men are six times more likely to develop problems achieving an erection after contracting the COVID-19 virus compared to men who didn’t get COVID. Other studies show a litany of symptoms caused by the coronavirus that can have an impact during sexual intercourse, including damage to the testis, testicular pain or swelling, difficulty achieving an orgasm, low libido, low testosterone levels, and even some urinary problems.
In this article, we’ll look at the main factors responsible for erectile dysfunction caused by COVID-19. We’ll also discuss how treatment at Cognitive FX helps patients recover from long COVID and may — although indirectly — represent a viable option to treat this symptom.
Our treatment is designed to help post-concussion patients recover from persistent symptoms. After just one week of treatment, 95% of our patients show statistically verified improvement in brain function. Thus far, we’ve seen similar results with long COVID patients who pass our current screening criteria. To discuss your specific symptoms of COVID-19 and determine whether you’re eligible for treatment at our clinic, schedule a consultation.
Note: Any data relating to brain function mentioned in this post is from our first generation fNCI scans. Gen 1 scans compared activation in various regions of the brain with a control database of healthy brains. Our clinic is now rolling out second-generation fNCI which looks both at the activation of individual brain regions and at the connections between brain regions. Results are interpreted and reported differently for Gen 2 than for Gen 1; reports will not look the same if you come into the clinic for treatment.
How Does COVID-19 Cause Erectile Dysfunction?
Male sexual arousal is a complex mechanism involving the brain, the nervous system, multiple muscles in the body, and blood vessels. Erectile dysfunction can occur due to problems with any of these components. For many men, erectile dysfunction has a strong physical component and is often associated with other health issues that increase the risk of ED, such as diabetes or cardiovascular disease. For others, there is no physical impediment to having an erection, but erectile dysfunction occurs due to psychological issues, such as stress and anxiety.
In fact, when the first reports about sexual dysfunction in COVID long haulers started appearing, most doctors assumed it was the result of stress caused by confinement and isolation. However, some patients weren’t feeling particularly anxious or stressed; nevertheless, the symptom persisted for months, which suggested a physical explanation.
It can be challenging to separate physical and psychological reasons for erectile dysfunction in COVID long haulers. At Cognitive FX, we find that concussion patients who have lived with similar symptoms for years have learned to recognize patterns in their symptoms. For example, if they experience erectile dysfunction during a bout of depression, it might have a psychological cause rather than a physical one (or could be a combination of both). In contrast, many long haulers have only lived with their symptoms for a few months, and it’s harder for them to “interpret” symptoms.
Briefly, there are four COVID-related factors that may lead to erectile dysfunction:
● Endothelial dysfunction
● Dysfunction in the autonomic nervous system (ANS), including cardiovascular and pulmonary issues
● Psychological issues aggravated by the pandemic
● Other causes (such as endocrine dysfunction)
We also briefly cover a few other factors that may cause sexual problems, but our list is not exhaustive. If you’re experiencing this issue—whether related to COVID-19 or not—we recommend you visit your family doctor or urologist as soon as possible.
Erectile Dysfunction as a Consequence of Endothelial Dysfunction
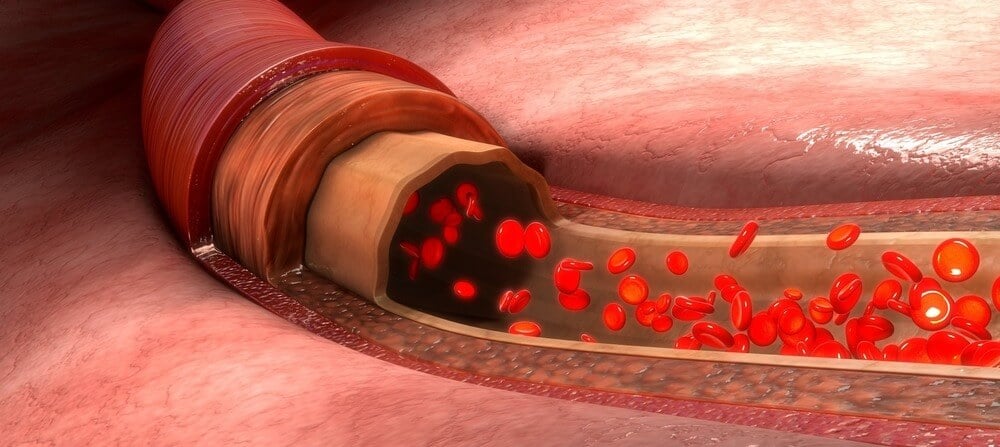
Every blood vessel in the body is lined with a single layer of cells called endothelial cells. Under normal circumstances, these cells play a vital role regulating the dilation and contraction of blood vessels to ensure enough blood flows where it’s needed.
In addition, the endothelium also protects internal organs from toxic substances, regulates the blood clotting mechanism, and controls inflammatory responses in the surrounding tissues. In short, a smooth running of the endothelium is critical for the normal functioning of the body’s tissues and organs.
However, this perfectly balanced system is disrupted in long COVID patients, as endothelial cells (which have ACE2receptors) are one of the most critical targets of SARS-CoV-2. There is enough evidence now to show that this virus causes endothelial dysfunction, leading to vascular leakage, thrombosis, blood clots, and an exaggerated inflammatory response.
This kind of vascular damage is the most likely explanation behind poor sexual performance and erectile dysfunction in long haulers. Erections rely solely on blood flow, so anything that interferes with the arteries’ ability to deliver blood to the penile tissue to create an erection could lead to erectile dysfunction. As the penis is one of the most vascular organs in the body, it’s not surprising that endothelial dysfunction caused by long COVID can lead to this kind of problem.
Disruption of the Autonomic Nervous System Also Causes Erectile Dysfunction
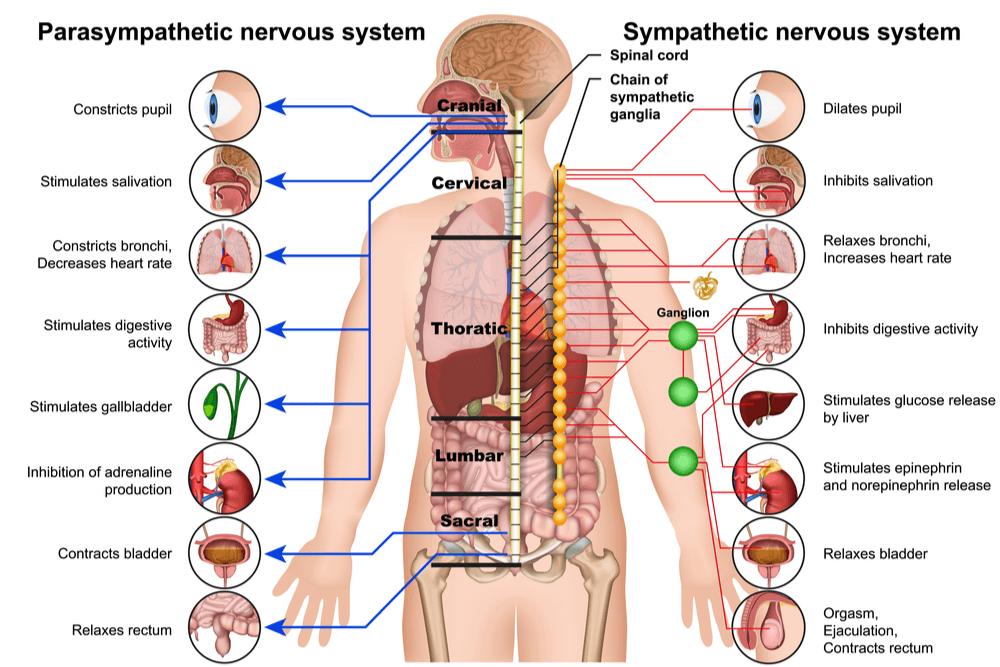
All the vascular events described above to ensure that an erection can occur are carefully orchestrated by the autonomic nervous system (ANS).
Recent studies show that the initiation, maintenance, and rigidity of penile erection are controlled by two sections of the ANS known as the parasympathetic nervous system (PNS) and sympathetic nervous system (SNS). To start, the PNS increases blood supply to the spongy tissues in the penis to allow an erection to occur. As sexual arousal increases, the SNS takes over until ejaculation.
Not surprisingly, any disruption in this balance between PNS and SNS causes erectile problems. In fact, a study reported approximately 14% of COVID long haulers experienced some sort of sexual impairment, along with a variety of other health problems also caused by ANS disruption, including pulmonary, urinary, and digestive conditions.
Erectile Dysfunction and the Stress Caused by the Pandemic
The psychological effects of the COVID-19 pandemic, including stress caused by job uncertainty and prolonged periods of staying at home, can also contribute to erectile dysfunction. Often, patients may wake up with an erection, but when it’s time to be intimate, they struggle. For these patients, the problem is either partially or wholly psychological.
While only a minority of people are affected by severe psychological trauma, it’s not unreasonable to suggest that most people have experienced some degree of distress and anxiety during the months of isolation. Since sexual activity is closely associated with mental health, sexual desire and frequency have declined during this pandemic, further aggravating the risk of erectile dysfunction.
Other Causes of Erectile Dysfunction after a COVID-19 Infection
There are several other factors related to COVID that can cause erectile dysfunction:
● Low oxygen levels: A COVID infection can lead to lung damage and low oxygen levels in the blood, which can, in turn, result in erectile dysfunction.
● Low testosterone: It’s common for long COVID patients to have reduced testosterone levels, typically accompanied by low production of sperm. This may cause low libido and erectile dysfunction.
● Fatigue and other long COVID symptoms: If you feel tired or are battling with constant headaches, you may find it difficult to engage in any sexual activity.
● Treatment for COVID: Patients staying in the ICU during a severe COVID case may receive many different medications, including thiazide-type diuretics, aldosterone receptor blockers, β-adrenergic receptor blockers, or ACE inhibitors to control blood pressure. Some of these are associated with a high risk of erectile dysfunction, but symptoms usually go away when you stop taking the medication.
Post time: Oct-25-2022